Cancer: A major national concern
Visit profiles to view data profiles on chronic and disabling conditions and on young retirees and older workers.
Americans consistently rank cancer as one of the most important health problems facing the nation.(1) It is the second leading cause of death in the United States — more than 550,000 people will die from cancer this year.(2) Cancer is the most costly illness in the United States and people with cancer often have high out-of-pocket health care costs. It is also often physically and emotionally difficult for those living with it and for their care providers. People who say they have had cancer are more likely to report poor health and symptoms of depression. Despite the fact that cancer is an important health problem, many Americans don’t comply with cancer screening protocols or take preventive measures such as protecting themselves from the sun.
The National Cancer Institute estimates that some 8.9 million Americans have a history of cancer.(3) This Profile examines people who report they have ever had cancer — referred to as “people reporting cancer” or “people with cancer.” People who do not report ever having cancer are referred to as “people not reporting cancer” or “people without cancer.” The population reporting cancer is somewhat different from the population of people in cancer registries because men are less likely than women to self-report and racial minority groups are under-represented.(4) Cancer registries also include those who have died from cancer.(5)
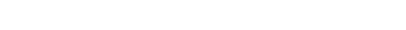
Expenditures are higher for cancer than for other conditions
Medical expenditures for cancer in 1996 were almost $10 billion higher than for the next most costly condition — trauma-related disorders. In 2001, overall costs for cancer were reported to be in excess of $156 billion. Medical expenditures account for about one-third — $56.4 billion — of the total. Lost productivity accounts for the majority of costs — $15.6 billion due to illness and $84.7 billion due to premature deaths.(6)
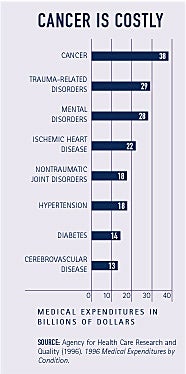
Cancer is associated with high out-of-pocket expenditures
Annual out-of-pocket expenditures for people with cancer are more than three times higher than those for people without cancer — $1,061 compared to $375. These additional expenditures may be particularly burdensome for the low-income population who pay a higher proportion of income for medical care. Among people with cancer, those with an annual family income under $20,000 spend 9 percent of their income on health care. By contrast, those with cancer who have an annual family income of $55,000 or more only spend about 1 percent of their income on health care (see Figure 1).
Prescription drugs contribute to high out-of-pocket expenditures
Some 90 percent of people who report they have ever had cancer say they have filled prescriptions in the last year compared to 57 percent of people not reporting cancer. Moreover, of those taking prescription drugs, people with cancer fill almost twice as many prescriptions — 21 compared to 11 for people without cancer.
Higher out-of-pocket expenditures for people with cancer compared to those without cancer likely reflects their more frequent use of prescription drugs. The cost difference between people with and without cancer is particularly large for the population under age 65, a group that generally tends to fill fewer prescriptions (see Figure 2).

WHAT IS CANCER?
Cancer is a family of diseases caused by uncontrolled growth of abnormal cells in a part of the body. Cancer is caused by both external factors (tobacco, chemicals, radiation, and infectious organisms) and internal factors (inherited mutations, hormones, immune conditions, and mutations that occur from metabolism). This uncontrolled growth often spreads beyond the original site, a process known as metastasis. When cancer metastasizes, the cancer is still defined by the original site. For example, colon cancer that has spread to the brain is still colon cancer.(7)
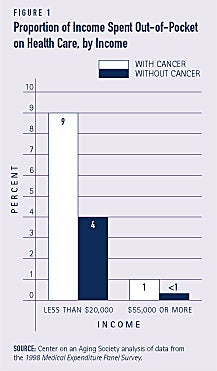
Skin cancer is the most common form of cancer
Of those reporting cancer the most frequently mentioned type is skin, including basal cell, squamous cell, and melanoma. Other commonly mentioned types of cancer are breast, prostate, uterine, cervical, and colorectal, which includes cancers of the colon and the rectum (see Figure 3). Lung cancer, one of the most common forms of cancer according to cancer registries, is not frequently mentioned. This is probably because it is the most deadly type of cancer — lung cancer accounts for 28 percent of cancer deaths but only 13 percent of diagnoses.(8)
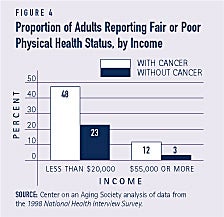
Poor health is associated with cancer, especially for the low-income population
People with cancer are more likely than those not reporting a history of cancer to describe their physical health status as fair or poor — 27 percent compared to 11 percent. Among the low-income population, this difference is even more pronounced — almost half of people with cancer say they are in fair or poor health compared to less than one-quarter of people without it (see Figure 4). Only 12 percent of people with annual incomes of $55,000 or more who have cancer report fair or poor health status.
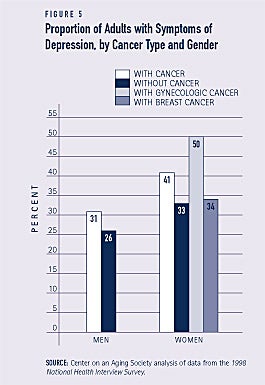
Symptoms of depression commonly accompany cancer
Generally, women are more likely than men to experience symptoms of depression. This is also true among the population reporting cancer — some 41 percent of women with cancer compared to 31 percent of men with cancer have experienced symptoms of depression within the last 30 days. Among women with cancer, rates differ depending on the type of cancer. For example, half of women with ovarian, cervical or uterine cancers report symptoms of depression. However, only 34 percent of women with breast cancer report symptoms of depression, a rate comparable to women who do not have cancer (see Figure 5).
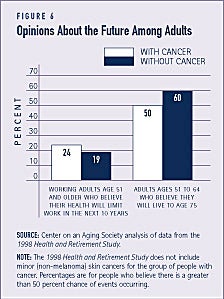
People with cancer are somewhat less optimistic about their future
Older adults with cancer are somewhat less optimistic about their future than those without cancer. For example, people ages 51 to 64 with cancer are less likely to believe they will live to age 75 than those who do not have cancer — 50 percent compared to 60 percent. Of those who are working, people with cancer are more likely to believe their health will limit their ability to work in the future (see Figure 6).
WHO GETS CANCER?
Men have a higher risk than women of developing cancer, and the occurrence of cancer increases with age. Among racial groups, African-Americans have higher rates of cancer and are about one-third more likely to die from it than whites.
Some people are at higher risk of developing cancer due to hereditary factors. For example, women with a mother or sister who has had breast cancer are at greater risk than women with no family history. Environmental factors, including tobacco use, poor dietary habits, infectious diseases, chemicals, and radiation cause an estimated 75 percent of all cancer cases and approximately one-third of cancer deaths. In particular, tobacco use is related to several types of cancer, including lung, mouth, and larynx.(9)
Cancer screening rates are far below future goals, even for those reporting a history of cancer
There are effective screening options for about half of all new cancers. Early detection can save lives, reduce the invasiveness and extent of treatment, and increase the chance of survival. In 1999 the American Cancer Society established nationwide objectives for the proportion of Americans being screened for specific types of cancer by the year 2015. Although a higher proportion of adults with cancer get screened compared to those without cancer, even they fall well below the future objectives (see Figure 7).
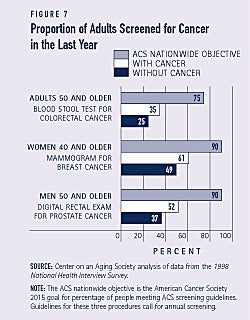
Blacks are less likely to be screened than whites. This could contribute to their higher death rates. It is likely the cancers are diagnosed at later stages. People in rural areas are less likely to be screened than those in urban areas. Only 20 percent of adults age 50 and older in rural areas say they have had a blood stool test in the last year compared to 28 percent of those in urban areas.
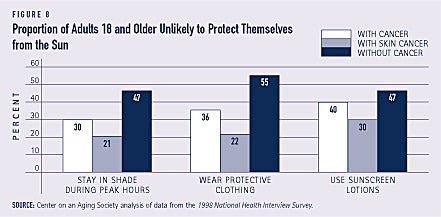
Many Americans don’t protect themselves from the sun
Despite the growing awareness that sun exposure is linked to skin cancer — the most common type of cancer — many Americans say they don’t wear protective clothing when in the sun, don’t stay in the shade during peak hours, and don’t use sunscreen or lotions. People who have had skin cancer are the most likely to protect themselves. Even so, more than 1 out of 5 say it is unlikely they take preventive measures while in the sun. About half of those who have never had cancer say they’re unlikely to protect themselves in the sun (see Figure 8).
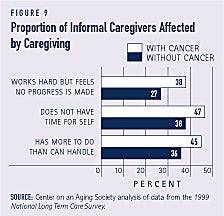
Caring for people with cancer affects caregivers
Informal caregivers of people with cancer are affected by the condition as well. Caregivers of people age 65 and older with cancer are more likely to report feeling overwhelmed, frustrated, strained and exhausted than caregivers of older persons without cancer (see Figure 9).
1. Blendon, R.J., Scoles, K., DesRoches, C., Young, J.T., Herrmann, M.J., Schmidt, J.L. Kim, M. (2001). “Americans’ Health Priorities: Curing Cancer and Controlling Costs.” Health Affairs, 20(6): 222-232.
2. American Cancer Society. (2002). Cancer Facts & Figures 2002. American Cancer Society: Atlanta, GA.
3. Ibid. Estimate does not include basal and squamous cell skin cancers.
4. Hewitt, M., Breen, N., Devesa, S. (1999). “Cancer Prevalence and Survivorship Issues: Analysis of the 1992 National Health Interview Survey.” Journal of the National Cancer Institute, 91(17): 1480-1486.
5. People who have had basal and squamous cell skin cancers are included in the group of people reporting cancer, but cancer registry statistics do not include them.
6. American Cancer Society. (2002).
7. Ibid. Also, American Cancer Society. Cancer Reference Information Fact Sheets. Available at www.cancer.org.
ABOUT THE DATA
Unless otherwise noted, the data presented in this Profile are from four national surveys of the United States civilian non-institutionalized population. The National Health Interview Survey (NHIS), conducted annually by the National Center for Health Statistics, is the principal source of information on the health of the U.S. population. The 1998 Medical Expenditure Panel Survey (MEPS), cosponsored by the Agency for Healthcare Research and Quality and the National Center for Health Statistics, provides national estimates of health care use, expenditures, sources of payment, and insurance coverage. The 1998 Health and Retirement Study (HRS) provides information about the population age 51 and older. HRS is sponsored by the National Institute on Aging and conducted by the Institute for Social Research at the University of Michigan. The 1999 National Long Term Care Survey (NLTCS) is conducted by the Center for Demographic Studies at Duke University and is sponsored by the U.S. Department of Health and Human Services. The NLTCS collects data on the community-dwelling population age 65 and older.
ABOUT THE PROFILES
This is the second set of Data Profiles in the series, Challenges for the 21st Century: Chronic and Disabling Conditions. The series is supported by a grant from the Robert Wood Johnson Foundation. This Profile was written by Susan Rogers with assistance from Lee Shirey and Laura Summer. Previous Profiles in the new series include:
1. Screening for Chronic Conditions: Underused services
2. Childhood Obesity: A lifelong threat to health
3. Visual Impairments: A growing concern as the population ages
The Center on an Aging Society is a Washington-based nonpartisan policy group located at Georgetown University’s Institute for Health Care Research and Policy. The Center studies the impact of demographic changes on public and private institutions and on the economic and health security of families and people of all ages.