Disease Management Programs: Improving health while reducing costs?
Visit profiles to view data profiles and issue briefs from the series Challenges for the 21st Century: Chronic and Disabling Conditions as well as data profiles on young retirees and older workers.
People with chronic conditions generally use more health care services, including physician visits, hospital care, and prescription drugs.(1) Increases in the number of people living longer with chronic conditions coupled with rising health care expenditures have spurred health plans, employers, and the government to look for ways to reduce health care use and costs. Disease management is one approach that aims to provide better care while reducing the costs of caring for the chronically ill. Disease management programs are designed to improve the health of persons with specific chronic conditions and to reduce health care service use and costs associated with avoidable complications, such as emergency room visits and hospitalizations.(2)
Substantial reductions in health care service use and expenditures have occurred for many individuals enrolled in disease management programs. Disease management is still relatively new, however, and programs are still evolving. There- fore, the long-term impact of this approach is not known.
Disease management programs are becoming more popular
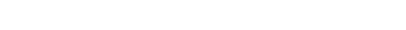
People with chronic conditions — 44 percent of non-institutionalized Americans — account for a disproportionate share — 78 percent — of health care expenditures in the United States.(3) This is true regardless of health insurance status (see Figure 1). Over the past decade, disease manage-ment has become an increasingly popular approach to caring for the population with chronic conditions in the United States.
WHAT ARE THE COMPONENTS OF DISEASE MANAGEMENT?
POPULATION IDENTIFICATION PROCESSES
As a first step, disease management programs need to identify a population, as well as how to enroll patients. Demographic characteristics and health care use and expenditures are generally reviewed to identify individuals who will benefit from a disease management program.
Programs are designed to target individuals with a specific disease. Costly chronic conditions, including asthma, diabetes, congestive heart failure, coronary heart disease, end-stage renal disease, depression, high-risk pregnancy, hypertension, and arthritis, have been the focus of these programs. Individuals with multiple conditions may also benefit from a disease management program. Enrollment in a program that targets the most severe disease necessitates attention to and coordination of care for other conditions.
EVIDENCE-BASED PRACTICE GUIDELINES
Physicians and providers within these programs are critical to educating patients on an ongoing basis about how to better manage their conditions. Many programs provide physicians with practice guidelines, based on clinical evidence, to ensure consistency in treatment across the targeted population.
COLLABORATIVE PRACTICE MODELS
Disease management generally entails using a multidisciplinary team of providers, including physicians, nurses, pharmacists, dieticians, respiratory therapists, and psychologists, to educate and help individuals manage their conditions. Health care providers may also work with support-service providers to fill in any gaps in the care team, such as the need for nutrition screening or remote-patient monitoring.
PATIENT SELF-MANAGEMENT EDUCATION
Disease management programs are based on the concept that individuals who are better educated about how to manage and control their condition receive better care. This could ultimately result in cost-savings. Program enrollees may need additional support to stick to their medical regimen. Counseling, home visits, 24-hour call centers, and appointment reminder systems have been used to support individuals who are managing their chronic conditions.(4)
PROCESS AND OUTCOMES MEASUREMENT
A method for the measurement of outcomes, including health care service use, expenditures, and patient satisfaction, must be determined prior to the start of the program. These measures are commonly compared to a baseline or a control group in order to measure the impact of the program.
ROUTINE REPORTING AND FEEDBACK BETWEEN PATIENTS, PROVIDERS, AND HEALTH PLANS
Routine reporting and feedback between patients, physicians, and other providers on the care team is often necessary to assure that patients are effectively managing their conditions and receiving the care they need. Additionally, health plans need feedback from patients and providers in order to evaluate their programs.
SOURCE: Disease Management Association of America.
HEALTH PLANS AND EMPLOYERS
Disease management programs have been developed and implemented largely by managed health care plans. Almost all health care plans have implemented at least one type of disease management program, and many have multiple programs (see Figure 2a). Programs for diabetes, asthma, and congestive heart failure are the most common (see Figure 2b). Health plans generally contract with vendors, also known as disease management organizations, to provide services. Some, however, choose to operate the program themselves.
Employer-sponsored disease management programs are relatively rare, but some employers are using these programs to improve the health of their workforce. Additionally, employers believe that disease management can increase worker productivity and reduce medical insur-ance costs. Between 1996 and 1998, use of disease management among a group of 375 employers, with some 12 million employees, increased from 31 percent to 43 percent.(5)
Some employers recognize that the disease management programs typically offered by health plans may not be appropriate for their workforce and, therefore, have invested substantial resources in developing programs that reflect their workers’ needs. For example, two large private employers with a younger workforce found that high-risk pregnancies were more prevalent than the conditions being targeted by their health plans’ programs. Thus, they worked with their health plans to implement programs that better meet the health care needs of their workforce.(6)

GOVERNMENT PROGRAMS
Almost half of states have implemented or are in the process of implementing Medicaid disease management programs. Similar to health plans, states can hire a disease management organization to administer the program, or they can create their own program. Although research on the impact of state Medicaid disease management programs is somewhat limited, there has been some evidence of improvements in the quality of care being provided and limited cost-savings.(7)
The Centers for Medicare and Medicaid Services (CMS) is currently conducting a series of disease management demonstration programs for Medicare beneficiaries with chronic conditions in traditional (fee-for-service) Medicare. CMS has contracted with disease management vendors, academic medical centers, and other provider-based programs to provide disease management services to fee-for-service beneficiaries with congestive heart failure, heart, liver, and lung diseases, diabetes, psychiatric disorders, Alzheimer’s disease or other dementia, and cancer.
In addition, about 11 percent of Medicare beneficiaries — 4.6 million — are enrolled in managed care plans.(8) Some of these plans operate disease management programs for conditions such as asthma, diabetes, depression, hypertension, and coronary heart disease.(9)
Disease management programs can reduce health care use and expenditures
Many disease management programs have been successful at improving self-care practices and reducing use of various health care services, including hospital admissions and emergency room visits. As a result, health care expenditures for certain populations with chronic conditions have decreased. Below are several programs that have improved self-care practices and reduced health care use and costs.
- Medicare beneficiaries in a diabetes management program improved many of their self-monitoring practices and used fewer inpatient services. Among some 6,800 beneficiaries, those enrolled in the program had a higher number of primary care physician visits, were more likely to receive eye, lipid, and kidney screenings, and had lower blood sugar levels, compared to those who were not enrolled in the program. In addition, program enrollees made fewer visits to the hospital and emergency room than non-enrollees. Over a two-year period, the average monthly cost per enrollee — $395 — was about 20 percent lower than per non-enrollee — $503.(10)
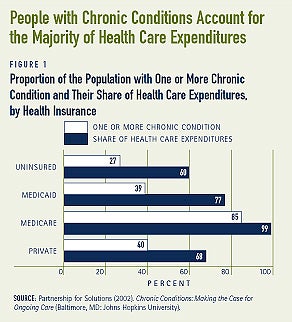
- Health care service use and expenditures decreased for about 7,000 people in a diabetes management program after one year. While enrolled in the program, individuals were more likely to receive tests to monitor their blood sugar, foot and eye exams, and cholesterol screenings. Compared to use prior to enrollment in the program, hospital admissions and bed days each decreased by about 20 percent. These outcomes likely contributed to total savings of $44 per month per enrollee (see Figure 3).
- Positive outcomes also occurred among 130 individuals in a diabetes management program. Within six months patients were more likely to receive hemoglobin tests and were less likely to show symptoms of hyperglycemia. Health care use, including physician visits, emergency rooms visits, and inpatient admissions, also decreased. An examination of pre-enrollment and post-enrollment costs, which included program costs, found that for every dollar spent on the patient, $4.34 were saved.(11)
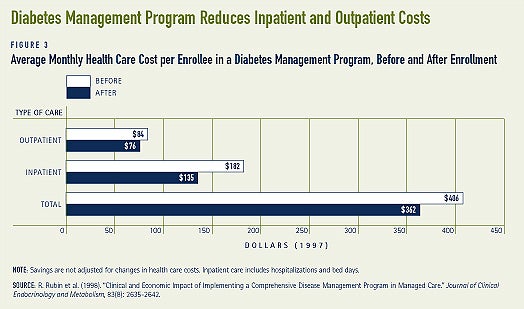
- Children (under age 21) enrolled in a pediatric asthma management pro- gram implemented by North Carolina’s Medicaid program used certain health care services less frequently. Children in the program had a 34 percent lower hospital admission rate and an 8 percent lower emergency room rate, compared to children not in the program. It also appears that efforts to increase awareness about the effectiveness of anti-inflammatory drugs were successful as pharmacy costs rose. Even with the increase in pharmacy costs, the average episode cost for children enrolled in the program was 24 percent lower than for non-enrollees (see Figure 4).
- Two years after enrolling in a disease management program for congestive heart failure, Florida Medicaid beneficiaries were monitoring their condition more closely and spending fewer days in the hospital. Beneficiaries were more likely to take prescription drugs to control their conditions and to receive an annual cholesterol screening. The number of days spent in the hospital decreased by 39 percent over the two-year period, and health care expenditures for the 2,500 beneficiaries decreased by 16 percent — a savings of $4.4 million after program costs.(12)
- People ages 40 and older with heart disease, lung disease, or arthritis enrolled in a six-month disease management program also used fewer health care services. Two years later, patients reported feeling less distressed about their health and that they were better able to manage their conditions. A reduction in outpatient visits, including emergency room and physician visits, and hospital stays reduced health care expenditures by $590 per participant over a period of two years. At a program cost of $70 to $200 per participant, the actual cost-savings ranged from $390 to $520.(13)
- Not all programs have been able to reduce health care service use, however. Several studies of asthma management programs found no substantial reductions in emergency room visits or hospitalization rates.
- For example, an 18-month study of an asthma management program for about 300 children in Colorado did not find any impact on their use of certain health care services. Emergency room visits and hospitalization rates of children in the program did not differ from those of children who were not in the program. However, children enrolled in the program were more likely than the other children to receive drugs that allow them to manage their condition more effectively.(14)
Long-term cost-savings remains to be seen
While many programs have succeeded at reducing health care expenditures, the potential for long-term savings is still not known. This is due, in part, to the fact that to date, studies that have found substantial cost-savings are generally confined to a short duration of time, and are typically based on the experiences of a single plan or program or are restricted to certain areas of the country.(15) Savings also vary across chronic conditions. A health plan in Seattle, for example, found that only one of its programs — a prenatal care program for high-risk pregnancies — produced a positive return on investment and improved patient outcomes. The other programs were costly to administer and did not serve many members.(16) Disease management programs are still relatively new and it is too early to determine whether or not they are cost-effective in the long-run.
Quality of life outcomes vary across programs
Measures of quality of life include those related to health or functional status, such as mobility, presence of symptoms, and overall energy level. Quality of life is more subjective, and can be influenced by one’s confidence in their health and by their ability to control the condition affecting them. Disease management has resulted in some improvements in the quality of life for people with chronic conditions.
- Individuals age 50 and older with chronic obstructive pulmonary disease in a disease management program experienced limited improvements in their health after a year. For example, while there was no improvement with respect to their lung capacity or their ability to walk for a 6-minute period, their social, emotional, and psychological well-being did improve.(17)
- Changes in the quality of life for another group of people age 70 and older in a congestive heart failure program were observed within a few months. Compared to people who were not in the program, those in the program were more likely to report less fatigue and better emotional status and control over their condition.(18)
- Improvements in the health and quality of life of adults in an asthma management program were small. For example, within one year the proportion reporting a decrease in their symptoms increased by less than 5 percent, from about 72 percent to 76 percent. Similarly, small improvements in their ability to function with asthma and their energy level were reported.(19)
Patient satisfaction is high
Results from the Community Tracking Study — a longitudinal study consisting of site visits to twelve nationally representative communities every two years — found that while health plans cannot be certain about the impact of disease management on health outcomes and costs, they are confident that the programs improve the satisfaction of members who participate in them.(20) Several other studies have found high patient satisfaction.
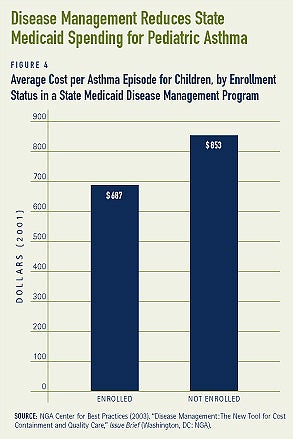
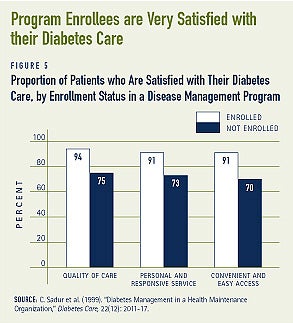
- Over 90 percent of individuals enrolled in a six-month diabetes management program were satisfied with the care they received for their condition. Proportions of enrollees who reported that the diabetes care they received was either “very good” or “excellent” were somewhat larger compared to people who were not enrolled in the programs. For example, some 94 percent of enrollees and 75 percent of non-enrollees were satisfied with the quality of diabetes care received (see Figure 5).
- A diabetes management program that reduced health care use and expenditures measured the satisfaction of both patients and physicians with the program. Some 45 percent of patients “strongly agreed” that they would recommend the program to others needing similar care, while some 29 percent reported that they “somewhat agreed.” An overwhelmingly majority of physicians who participated in the program were also satisfied with the program. For example, 90 percent of physicians thought that the overall quality of care provided was good to excellent, and 85 percent thought that the program provided better care to the patients.(21)
Program participation and compliance are universal challenges
Disease management requires individ- uals to commit a substantial amount of time and effort to improving their health care practices. Thus, patients need to be encouraged to enroll in a program. Communicating the benefits of disease management is one way to do this. Another common challenge for disease management is low patient compliance. Patient compliance ranges widely among populations with different chronic conditions. Some patients are set in their ways and find the care plans oppressive, while others may not fully trust the program.(22) Financial incentives may be needed to encourage both program participation and compliance. Some programs offer extra benefits, reduced co-payments, free supplies, or discount vouchers for disease-specific supplies.(23)
Financial incentives may also be needed to encourage provider participation. Because a main goal of disease management is to reduce health care service use, decreases in revenue may be a concern for some providers. Some health plans reward providers for their efforts with extra payments. Blue Cross of California, for example, awards physicians who meet nationally recognized quality guidelines with a modest financial bonus.(24)
Communication barriers between patients and providers pose challenges. Cultural differences, as well as language barriers, can inhibit program outcomes. Furthermore, because disease management requires both patients and providers to closely monitor the condition being treated, it is important that both parties are easily accessible. Communication via email has become increasingly common, though it is not an option for everybody. Email also allows physicians to address patients’ non-urgent medical questions.(25)
Providers in a coordinated care team also need to be able to communicate effectively. Systems that allow providers to easily share information with each other, including patient health status, clinical information, and case management notes, help keep the lines of communication open, and ultimately benefit the patient.(26)
Conclusion
As more people live longer with costly chronic conditions, there are likely to be more disease management efforts. As programs and technology evolve, disease management could become more effective and efficient at helping people with chronic conditions.
1. Partnership for Solutions (2002). Chronic Conditions: Making the Case for Ongoing Care (Baltimore, MD: Johns Hopkins University).
2. Bodenheimer, T. (1999). “Disease Management — Promise and Pitfalls,” The New England Journal of Medicine, 240(15): 1202-1205.
3. Partnership for Solutions (2002).
4. NGA Center for Best Practices (2003). “Disease Management: The New Tool for Cost Containment and Quality Care,” Issue Brief (Washington, DC: NGA).
5. Pharmacy Benefit Management Institute (1999). Wyeth-Ayerst Prescription Drug Benefit Cost and Plan Design Survey Report, 1999 Edition.
6. Short, A., G. Mays, and J. Mittler (2003). “Disease Management: A Leap of Faith to Lower-Cost, Higher-Quality Health Care,” Issue Brief, No. 69 (Washington, DC: Center for Studying Health System Change).
7. NGA Center for Best Practices (2003).
8. Dallek, G., B. Biles, and L. Hersch Nicolas (2003). “Lessons from Medicare+Choice for Medicare Reform,” Policy Brief (New York, New York: The Commonwealth Fund).
9. Draper, D., A. Cook, and M. Gold (2003). How Do M+C Plans Manage Pharmacy Benefits? Implications for Medicare Reform (Washington, DC: Kaiser Family Foundation).
10. Sidorov, J. et al. (2002). “Does Diabetes Disease Management Save Money and Improve Outcomes?,” Diabetes Care, 25(4): 684-689.
11. Berg, G. and S. Wadhwa (2002). “Diabetes Disease Management in a Community-Based Setting,” Managed Care, 11(6):42, 45-50.
12. Statement of Christobel Selecky, President-elect of the DMAA, “Evaluating Coordination of Care in Medicaid: Improving Quality and Clinical Outcomes,” before the House Committee on Energy and Commerce Health Subcommittee, October 15, 2003.
13. Lorig, K. et al. (2001). “Chronic Disease Self-Management Program,” Medical Care, 39(11): 1217-1223.
14. Lukacs, S. et al. (2002). “Effectiveness of an Asthma Management Program for Pediatric Members of a Large Health Maintenance Organization,” Archives of Pediatric Adolescent Medicine, 156: 872-876.
15. AAHP/HIAA (2003). The Cost Savings of Disease Management Programs: Report on a Study of Health Plans (Washington, DC: AAHP/HIAA).
17. Bourbeau, J. (2003). “Reduction of Hospital Utilization in Patients with Chronic Obstructive Pulmonary Disease,” Archives of Internal Medicine, 163: 585-591.
18. Rich, M. et al. (1995). “A Multidisciplinary Intervention to Prevent the Readmission of Elderly Patients with Congestive Heart Failure,” The New England Journal of Medicine, 333(18): 1190-1195.
19. Belman, M. (2003). “An Asthma Management Program in Managed Care,” Managed Care, Supplement, 12(1): 18-21.
20. Felt-Lisk, S. and G. Mays (2002). “Back to the Drawing Board: New Directions in Health Plans’ Care Management Strategies,” Health Affairs, 21(5): 210-217.
21. Rubin, R. et al. (1998). “Clinical and Economic Impact of Implementing a Comprehensive Disease Management Program in Managed Care,” Journal of Clinical Endocrinology and Metabolism, 83(8): 2635-2642.
22. Adonmeit, A., A. Baur, and R. Salfeld (2001). “A New Model for Disease Management,” The McKinsey Quarterly, Autumn.
23. Atkinson, W. (2002). “Making Disease Management Work,” HRMagazine, January.
25. Patt, M. et al. (2003). “Doctors Who Are Using E-mail with Their Patients: a Qualitative Exploration,” Journal of Medical Internet Research, 5(3):e9.
26. Mechanic, R. (2002). “Disease Management: A Promising Approach for Health Care Purchasers,” Executive Brief (Washington, DC: National Health Care Purchasing Institute).
ABOUT THE ISSUE BRIEFS
This is the fourth in a series of Issue Briefs on Challenges for the 21st Century: Chronic and Disabling Conditions. This series is supported by a grant from the Robert Wood Johnson Foun-dation. Lee Thompson wrote this Issue Brief.
The Center on an Aging Society is a non-partisan policy group located at Georgetown University’s Institute for Health Care Research and Policy. The Center studies the impact of demographic changes on public and private institutions and on the financial and health security of families and people of all ages.